In industries like medical device production and the packaging of other sensitive products, maintaining the highest levels of cleanliness is critical. These products are used in environments where contamination can cause serious harm, such as medical procedures, surgeries, or sensitive treatments. To prevent any risk of contamination, filling processes are often carried out in ultra-clean environments, such as clean rooms, where the atmosphere is carefully controlled. This article explores the importance of ultra-clean environments in filling processes, especially in medical device production, and discusses the necessary standards, technologies, and sterilization techniques that must be followed to ensure the safety and quality of these products.
What is An Ultra-Clean Environment And For Which Products is It Necessary?
An ultra-clean environment refers to a controlled setting where the levels of airborne particles, contaminants, and microorganisms are kept to an absolute minimum. These environments are designed to protect products from contamination during manufacturing, packaging, and filling processes.
Ultra-clean environments are essential in industries where even the smallest contamination can result in severe health risks or product failure.
Creating and maintaining such an environment requires meticulous control over factors like air quality, temperature, humidity, and personnel access, all of which play a significant role in preserving the sterility of the products.
How Does The Filling Process Work in Clean Rooms For Medical Devices?
In clean rooms, the filling process for medical devices involves a series of steps designed to ensure the sterility of the product and prevent any contamination. These clean rooms are equipped with advanced filtration systems and controlled airflow to keep the air free of particulates, bacteria, and other potential contaminants.
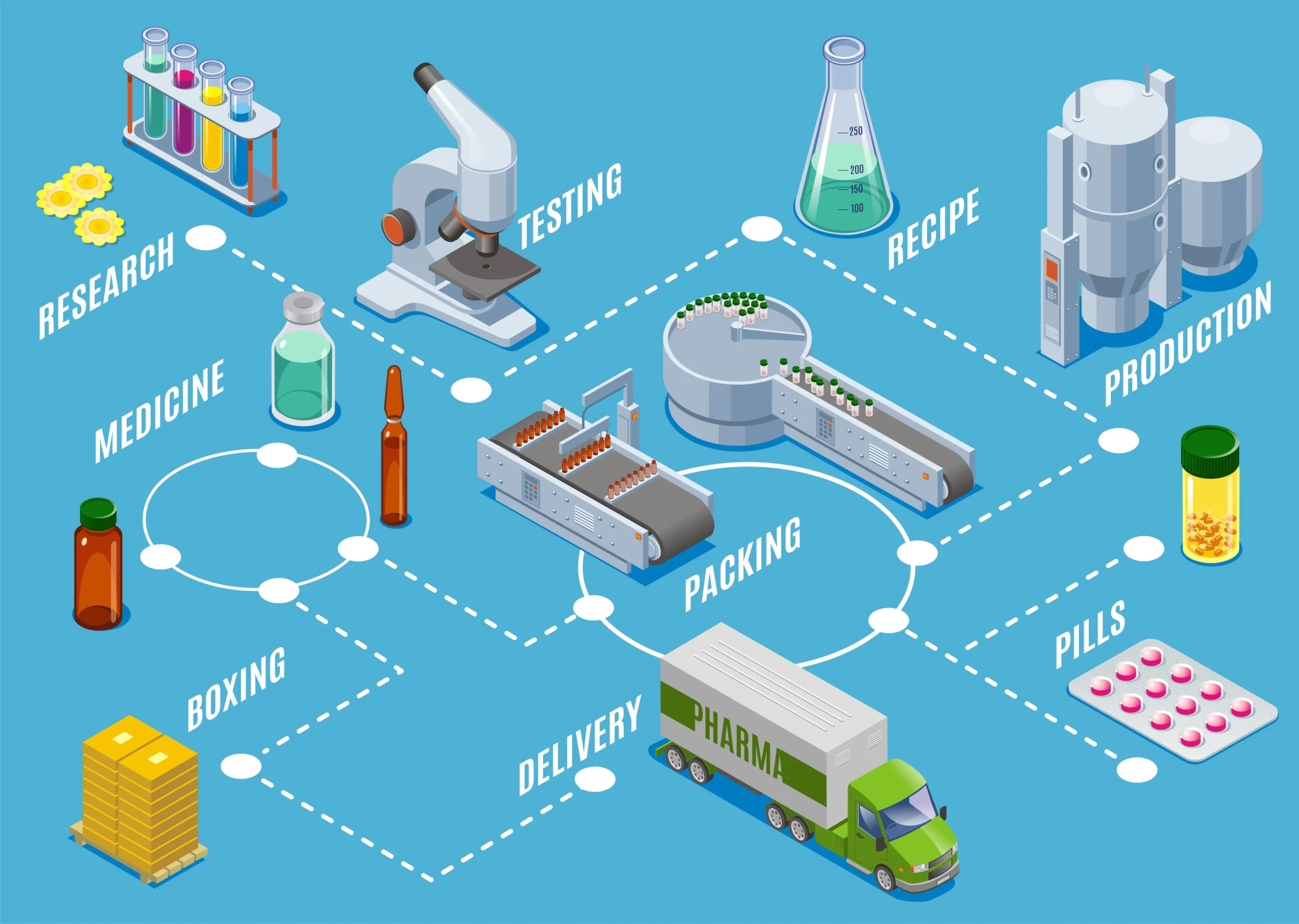
The filling process begins with the sterilization of the medical device and its components. After sterilization, the device is placed in a controlled area where any necessary liquids or gels are filled into the device under strict cleanliness conditions. For example, if filling syringes with medicine or other injectable substances, the process must be conducted in an environment that ensures no particles or microbes are present.
The entire process, from the preparation of materials to the final sealing of the product, is carried out in an environment where operators must follow strict hygiene protocols. This includes wearing personal protective equipment (PPE), such as gloves, gowns, face masks, and sometimes even full-body suits, to prevent contamination.
Which Technology is Used in Filling Processes Requiring An Ultra-Clean Environment?
In filling processes requiring ultra-clean environments, several advanced technologies are used to ensure product sterility and prevent contamination. One of the most important technologies is High-Efficiency Particulate Air (HEPA) filtration systems, which are capable of trapping airborne particles as small as 0.3 microns. These filters are crucial in maintaining the air quality of clean rooms, ensuring that contaminants do not settle on products during the filling process.
Additionally, ultraviolet (UV) sterilization technology is commonly used in clean rooms to further ensure that the environment remains free from harmful microorganisms. UV light is effective in neutralizing bacteria, viruses, and other pathogens that might be present in the air or on surfaces.
For the filling machines themselves, automated systems with advanced controls are used to monitor and regulate factors like temperature, pressure, and the filling rate. This technology helps maintain consistent quality while reducing the risk of human error. In some cases, robotic systems are employed to handle sensitive materials, further minimizing the chances of contamination.
How Are Clean Room Standards And Regulations Applied in Medical Device Production?
Clean room standards and regulations are essential in medical device production to ensure that products meet safety and quality requirements. These standards, often set by regulatory bodies like the International Organization for Standardization (ISO), outline specific guidelines for cleanliness, air quality, and operator behavior in clean rooms.
One of the most widely followed standards is ISO 14644, which defines the classification of air cleanliness in terms of particulate contamination. Clean rooms are classified into different categories based on the allowable number of particles per cubic meter of air, with the highest standard being Class 1, which allows only 1 particle per cubic meter.
Regulations also specify requirements for the design and construction of clean rooms, including the type of materials used for walls, floors, and ceilings, which must be non-porous and easy to clean. The HVAC (heating, ventilation, and air conditioning) systems must be capable of maintaining proper air pressure and filtering out contaminants effectively.
Strict guidelines are also in place for personnel working in clean rooms. Operators must be properly trained and equipped with suitable PPE to minimize the risk of introducing contaminants. They must also follow strict protocols for entering and exiting clean rooms, including gowning procedures and hand sanitization.
Which Sterilization Techniques Are Suitable For Filling in A Clean Environment?
Sterilization is a critical component of filling processes in clean environments, especially when dealing with medical devices. The most common sterilization techniques used in these settings include:
- Autoclaving (Steam Sterilization): This is one of the most effective methods for sterilizing medical devices and packaging materials. It uses high-pressure steam to kill bacteria, viruses, and other pathogens. Autoclaving is particularly useful for heat-resistant materials.
- Gamma Radiation: Gamma radiation is another sterilization method often used in clean environments. It involves the use of high-energy radiation to kill microorganisms and sterilize medical devices. Gamma radiation is ideal for items that cannot withstand heat but need to be sterilized effectively.
- Ethylene Oxide (EtO) Sterilization: EtO sterilization is a gas-based method that is used for heat-sensitive products. It is widely used in the sterilization of medical devices and equipment that would be damaged by other forms of sterilization.
- UV-C Sterilization: Ultraviolet light (UV-C) is used to disinfect surfaces and air in clean rooms. It is an effective way to reduce microbial contamination and maintain the sterility of the environment.
These techniques are used depending on the specific requirements of the product being filled and the materials involved
What Measures Should Be Taken To Prevent Contamination Of Contents With Microorganisms?
Preventing contamination with microorganisms during the filling process is a critical aspect of working in an ultra-clean environment. Several measures must be taken to ensure the contents remain sterile:
- Air Filtration: HEPA and ULPA filters should be used to keep the air free from particles, dust, and microorganisms.
- Sterilization of Equipment: All equipment used in the filling process, including machines and containers, must be sterilized before use to prevent contamination.
- Personnel Hygiene: Workers must undergo thorough hygiene procedures, such as hand washing and wearing protective gear, before entering clean rooms.
- Minimizing Human Interaction: The less human contact a product has, the lower the risk of contamination. Automated systems and robots can be used to handle materials and products to reduce the chances of contamination.
- Sealing and Packaging: Once the product is filled, it should be sealed immediately to prevent exposure to the outside environment. Packaging materials should also be sterilized before use.
How is Sterility Control Ensured For Equipment And Filling Machines Operating in An Ultra-Clean Environment?
Ensuring sterility in equipment and filling machines is essential for preventing contamination. This is achieved through regular cleaning and sterilization procedures, as well as by using sterilizable materials in the construction of equipment.
Filling machines used in clean rooms are often designed with features that facilitate easy cleaning and maintenance. For example, machines may have smooth surfaces and minimal joints, which reduces the risk of contamination. They should also be equipped with sensors to detect any deviations from the required sterile conditions.
Additionally, all equipment should be regularly tested for sterility, with periodic checks conducted to ensure that no bacteria or contaminants are present.
What Steps Should Be Followed To Ensure The Cleanliness And Safety Of Materials Used in Medical Device Production?
The materials used in medical device production, including packaging and components, must be thoroughly cleaned and sterilized before being used in the manufacturing process. To ensure cleanliness and safety, the following steps should be followed:
- Material Selection: Use materials that are resistant to contamination and can withstand sterilization methods, such as autoclaving or radiation.
- Cleaning Protocols: All materials must be cleaned according to strict protocols before use. This may involve washing, disinfecting, and drying to remove any potential contaminants.
- Sterilization: After cleaning, materials must be sterilized using an appropriate method, depending on their characteristics and the type of product being produced.
- Storage and Handling: Materials should be stored in a controlled environment to prevent contamination. They should also be handled with care to avoid exposure to contaminants.
What is The Importance Of Air Filtration And Circulation Systems For The Clean Room Environment?
Air filtration and circulation systems are essential for maintaining the sterility of a clean room. These systems work together to control the flow of air and prevent contaminants from entering the environment.
HEPA and ULPA filters are used to remove particles from the air, ensuring that only clean, filtered air enters the clean room. The circulation systems maintain positive air pressure, which prevents unfiltered air from entering the room.
Proper airflow also ensures that any contaminants are quickly removed, reducing the risk of contamination during the filling process.
How Are Quality Control And Validation Processes Applied in The Production Process?
Quality control and validation are integral to ensuring that products produced in clean environments meet the necessary safety and quality standards. Validation processes involve verifying that the clean room, equipment, and sterilization methods are functioning as intended.
Regular quality checks, including microbial testing and visual inspections, are performed throughout the production process to identify any issues that could compromise product safety. Additionally, the entire process must be documented to ensure compliance with regulatory standards.
Filling processes that require ultra-clean environments are essential for the production of sensitive products such as medical devices. Read our other blog post to discover how these rigorous standards intersect with safety and compliance regulations in general aerosol production.